The UK is often referred to as the 'sick man of Europe’. And at first glance the description may seem merited. Just last month the Organisation for Economic Co-operation and Development (OECD) revealed that life expectancy here is the lowest in Western Europe.
This follows a 2020 Public Health England report which found that, while we compared well against the US, we lag behind European nations such as Spain, the Netherlands and Scandinavian countries on rates of chronic illness, disability and death from poor health.
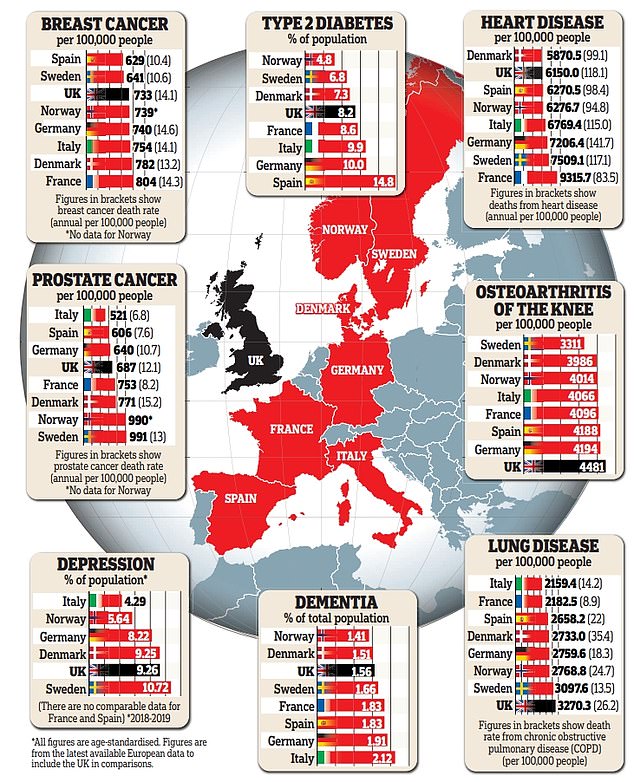
What’s more, our cancer survival rates are so far behind our European neighbours that patients with prostate, bowel, breast and cervical cancers in the UK today have the same chance of surviving as those in Sweden, Denmark and Norway did around two decades ago, according to the charity Macmillan Cancer Support.
On top of that, the UK has one of the highest obesity rates in Europe (only Turkey and Malta are worse).
And yet… it isn’t all bad news.
The UK leads the way in reducing smoking levels – and the NHS is one of the few healthcare systems providing free medication and check-ups for some people with chronic conditions, such as type 2 diabetes.
Here we look at how the UK really compares with Europe in tackling common conditions – and what could improve our ratings.

Just last month the Organisation for Economic Co-operation and Development (OECD) revealed that life expectancy in the UK is the lowest in Western Europe
Breast and prostate cancer
Survival rates for two of Europe’s most common cancers – breast and prostate – are lower in England, Wales and Scotland than the European average, according to Cancer Research UK.
One possible reason is that the UK has the least frequent breast cancer screening programme in Europe, offering women aged 50 to 71 a mammogram once every three years – the European average is once every two years – meaning British women risk being diagnosed later.
In Sweden, women have screenings every 18 to 24 months; 10.6 women per 100,000 in the population die of breast cancer a year compared with 14.1 in the UK (this difference will result from other factors, too, such as access to certain treatments).
Dame Lesley Regan, the women’s health ambassador for England, has criticised the three-year schedule for being dictated by 'budgets’ and 'not based on scientific evidence’.
With prostate cancer, the UK does not offer routine screening, although it is unclear whether doing so would help to save lives.
The current blood test used to detect the disease, the prostate specific antigen (PSA) test, has a high risk of false negative results, leading to men potentially undergoing further needless tests, or identifying cancers that don’t affect health or mortality.
Sweden has been trialling different screening tests since 2018, including using risk calculators to decide whether to give men fingerprick blood tests or MRI scans. Yet while diagnosis rates have increased, the death rates in Sweden remain higher.
Whereas in the UK, 687 men per 100,000 in the population are diagnosed with prostate cancer each year and 12.1 per 100,000 die, in Sweden 991 men per 100,000 are diagnosed, and there are 13.3 deaths. Why remains unclear.
Cancer survival rates have been boosted in some countries by investment in new treatments.
In Spain, the drug talazoparib, for late-stage breast cancer, has been available to patients since 2018 – but it only became available on the NHS in January this year.
The Spanish approach has appeared to pay dividends, even before the use of talazoparib: survival rates in women with advanced breast cancer rose from 36 per cent at the start of the 2000s to 43 per cent by the early 2010s – the UK five-year survival rate for stage 4 breast cancer is around 25 per cent.
Spain now has one of the lowest breast cancer mortality rates (10.4 deaths per 100,000 people, compared with 14.1 in the UK).
Spanish men can also access the hormonal therapy abiraterone to prevent prostate cancer spreading, while men in England and Northern Ireland can only have the treatment if their cancer is advanced (it is available in Scotland and Wales).
Spain’s prostate cancer death rate is 7.6 deaths per 100,000 people; it’s 12.1 per 100,000 in the UK.
Waits to start treatment can also be longer in the UK. A study by the International Cancer Benchmarking Partnership found UK patients with common cancers could wait up to five weeks longer to start treatment than those in Norway.

Dame Lesley Regan, the women’s health ambassador for England, has criticised the UK’s three-year cancer screening schedule for being dictated by 'budgets’ and 'not based on scientific evidence’
Depression
Rates of depression in the UK have been steadily rising. Five years ago, we ranked eighth across Europe, and now we’re second only to Sweden, according to the Lancet last year.
In fact, the comparison of 29 European countries based on data collected between 2018 and 2020 found that one in ten people in the UK lives with depression, up from one in 14 five years ago. This is more than other northern European countries, such as Iceland, and double the rate in Italy (one in 20 people).
And the situation may be even worse than these figures suggest. According to the Office for National Statistics (ONS), in 2022 one in six Britons had 'moderate to severe’ depression.
While one reason for the rise is changing attitudes towards mental health problems – so more people seek help – experts fear there are factors specific to Britain.
The ONS researchers found being chronically ill, an unpaid carer and having difficulties paying bills increased the chances of someone being depressed.
And while financial pressures due to the pandemic and the cost-of-living crisis hit other countries, too, 'it may be [these had] an outsized effect in the UK – perhaps because of difficulties in accessing NHS treatments, or the relatively low level of basic unemployment support in the UK,’ said research economist Eduin Latimer.
His recent report for the Institute for Fiscal Studies found that two in five new claims for health-related benefits are now for mental-health reasons.
The UK has more psychologists per head than Italy and Spain – 24.6 per 100,000 people, compared with 8.62 in Italy, although waiting times are much longer.
On average, people wait five months for a first appointment in the UK, but one to two months in Spain and less than a month in Italy, according to European investigative group Civio.
Type 2 diabetes
The number of Britons with type 2 diabetes has more than doubled in the past three decades and is increasing faster than most other European countries, according to a 2021 study by Imperial College London of the UK and EU nations.
This may be because type 2 diabetes is linked to obesity (three in ten people in the UK are obese). Yet, paradoxically, the UK rate (one in 12) is below countries such as Spain (one in seven), which has lower obesity rates, reports the International Diabetes Federation. It’s not clear why.
The UK has made more progress than most of its European neighbours in reducing diabetes-related deaths.
The study by Imperial found that deaths from diabetes have dropped by 47 per cent in the UK since 1990 – this was the biggest reduction in Europe in men and the second biggest in women. In Denmark and Eastern European nations death rates increased.
One reason for this is comprehensive and free NHS diabetes care.
In Germany, for example, patients must pay €5 to €10 for each insulin or diabetes medication prescription, while in the UK most people receive free insulin and other medications – as well as an annual diabetes check-up at their GP surgery or hospital, which includes medication reviews, tests and foot and eye health checks. Such reviews aren’t routinely offered in all European countries.
’Monitoring these things means any complications can be spotted and treated early, so people with diabetes are much less likely to develop long-term complications and more likely to live longer, healthier lives in the UK,’ says Professor Ketan Dhatariya, a consultant in diabetes, endocrinology and general medicine, and chair of the Association of British Clinical Diabetologists.
Dementia
Italy is the dementia capital of Europe, with around 2.12 per cent of the population having the condition, compared with 1.56 per cent in the UK, says Alzheimer Europe.
That’s due to higher life expectancies (age is the biggest risk factor for dementia) and low birth rates in Italy – nearly a quarter of the population is over 65.
By contrast, just under a fifth of the UK population is over 65.

Rates of depression in the UK have been steadily rising. Five years ago, we ranked eighth across Europe, and now we’re second only to Sweden
Compared with other European countries, the UK performs well in its treatment of dementia. It was one of the best for having multiple clinical trials under way and being ready to roll out new treatments, if any become available, according to the 2023 European Dementia Monitor report.
The UK was also ranked among the top countries for having dementia-inclusive initiatives and protecting the legal, care and employment rights of people with dementia (although Scotland scored higher than England).
A separate 2022 study by German researchers, which compared 17 European countries, found dementia patients could generally access similar levels of hospital care throughout the UK, whereas in countries such as Germany there is a postcode lottery.
But social care for dementia patients in the UK is held back by high levels of care staff vacancies and poor training, say experts.
In the UK, around nine in ten care homes are privately owned and care varies. But in Denmark nine in ten homes are state-owned and care is more standardised.
Heart disease
Rates of heart disease in the UK are slightly lower than the European average (6,150 per 100,000 people compared with 6,908 in Western Europe), reported the Journal of the American College of Cardiology in 2021.
As with similar European countries such as Sweden and Italy, the UK’s heart disease, heart attack and stroke rate dropped by around 30 per cent between 2000 and 2019 due to better awareness of the causes of heart disease (such as eating too much salt), earlier detection and better management of the condition.
But levels have risen by around 14 per cent since the pandemic – which may in part be due to a rise in heart disease triggered by Covid-19 infections.
And early deaths from the condition in the under-75s are increasing for the first time in almost 60 years across the UK.
Furthermore, while France has higher rates of heart disease (9,316 per 100,000 people) it has much lower death rates.
In the UK, 118 in every 100,000 people die from the condition each year, compared with 83.5 per 100,000 in France, likely due to differences in care.
’At every level, the system providing heart care for patients in the UK is damaged – from prevention and diagnosis through to treatment and crucial research,’ says Dr Sonya Babu-Narayan, associate medical director at the British Heart Foundation (BHF).
’We’ve seen record high waiting lists for cardiovascular care in England, while ambulance response times for heart attacks and strokes are also incredibly high [on average 42 minutes last month, up from 18 minutes before the pandemic].’
And, as of September, more than 9,000 people have been waiting for over a year for time-critical tests and treatment, compared with just 28 people in February 2020, according to the BHF.
Another factor is obesity – around 25 per cent fewer people in France are obese than in the UK.
Osteoarthritis
The UK has higher rates of osteoarthritis, the painful joint condition, than most other European countries, partly explained by our levels of obesity.
In the UK, 4,481 people per 100,000 live with knee osteoarthritis (the most common form) – around a third higher than the rate in Sweden (3,311 per 100,000). In Sweden, just 18 per cent of women and 23 per cent of men are obese – some of the lowest rates in Western Europe, compared with 28 per cent for both sexes in the UK.
And waits for treatment can also be longer here, too. The NHS says first-line treatment is exercise, which can be guided by a physiotherapist. But we have fewer physiotherapists per head of population than virtually every other major European nation.
In the UK, there’s one physiotherapist for every 1,136 people, whereas in Germany it’s one for every 430 people, according to the Chartered Society of Physiotherapy.
And while patients in Germany, for example, can book directly with an orthopaedic surgeon, in the UK you have to be referred, and only after trying physiotherapy or losing weight first.
This might explain why the annual rates of hip and knee replacement operations are high in Germany – at 309 and 223 per 100,000 people respectively.
By comparison the UK performs 181 hip and 145 knee replacements per 100,000 people annually, reports the Economist Intelligence Unit.
A patient in England now waits around 4.6 months for joint replacement surgery on average. This is slightly lower than in Spain (4.7 months) and Norway (5.4 months), but four times longer than the average wait in Italy of around 30 days, analysis by the Nuffield Trust think-tank found.
Waiting times soared during lockdown – before 2020, average waits were less than three months – and have not returned to pre-pandemic levels. But waits in Spain, for example, have remained largely stable.
’Waiting times were growing in England long before the pandemic began, and more resilient healthcare systems [in other countries] seem to have been better placed to stabilise and return to their pre-pandemic levels,’ says Sarah Reed, a senior fellow at the Nuffield Trust.
Lung disease
Chronic obstructive pulmonary disease (COPD), an umbrella term for diseases linked to damage to the lungs, is a particular problem here, with 1.4 million Britons diagnosed and an estimated further 500,000 undiagnosed.
The main trigger is smoking, but exposure to dust, fumes, chemicals and air pollution also increases your risk.
Surprisingly, although smoking rates in England are much lower than in France (a fifth of British men smoke, compared with a third of French men), we have much higher rates of COPD and deaths – 26.2 per 100,000 die of COPD in the UK each year, nearly triple the number (8.9) in France.
In fact, the UK has the highest death rate from lung conditions in Europe.
Some scientists believe diet is a factor: research suggests that people with COPD whose diet is high in fruit and vegetables, wholegrains and fish have better outcomes than those who eat lots of processed, sweet or fatty foods, cured meats and sweet drinks.
On average, less than a third of the typical French diet is made up of ultra-processed food, compared with more than half of the UK diet.
Another problem is delays in accessing treatment during flare-ups. A study comparing the UK and France, published in the journal BMJ Open Respiratory Research, found that patients here were more than twice as likely to end up in A&E with severe COPD symptoms than French patients, and nearly twice as likely to be hospitalised.
The researchers suggested this could be down to how quickly patients can see their GP.
Furthermore, less than a fifth of people diagnosed with COPD here receive the recommended levels of care, according to the charity Asthma + Lung UK.
Its clinical lead, Dr Andrew Whittamore, says it can take time for people to even get a COPD diagnosis due to 'poor access to spirometry testing [a simple breathing check for lung health]’.
He adds: 'And once diagnosed, many people are not receiving the basic care they need – such as help using inhalers and regular medication reviews.’